Goals of evaluation
The primary objectives of the medical evaluation of the first seizure are to establish whether the event was a seizure, and if so, whether it resulted from a correctable systemic process or whether the patient is at risk for developing further unprovoked seizures (epilepsy).
Definitions
Seizures are typically referred to as either acute symptomatic seizures or unprovoked seizures depending on the clinical circumstances at the time of the event.
Acute symptomatic seizure
An acute symptomatic seizure is a seizure that occurs in the setting of acute medical (eg, hypoglycemia, hyponatremia) or neurologic illness or injury (eg, stroke, traumatic brain injury, meningitis, anoxic encephalopathy). Such seizures may recur during the index illness but generally carry a low risk of future epilepsy compared with unprovoked seizures.
Unprovoked seizure – An unprovoked seizure refers to a seizure of unknown etiology as well as one that occurs in relation to a preexisting brain lesion or progressive nervous system disorder. Approximately one-third of adults with a first unprovoked seizure will have a recurrent seizure (ie, epilepsy) over the next five years.
Epilepsy
Epilepsy refers to the tendency for recurrent, unprovoked seizures.
Focal versus generalized onset
Seizures are further categorized as either focal or generalized according to whether the onset of electrical activity involves a focal region of the brain or the entire cortex simultaneously. The clinical manifestations of seizures vary based on the location of the seizure in the brain and the amount of cortex that is involved.
Causes
The causes of epilepsy can be broadly categorized as genetic, structural, metabolic, immune, infectious, and unknown. While a significant proportion of epilepsy in childhood has a genetic, metabolic, or congenital structural basis, epilepsy diagnosed in adults is more likely to be due to an acquired vascular, degenerative, or neoplastic etiology.
Differential diagnosis
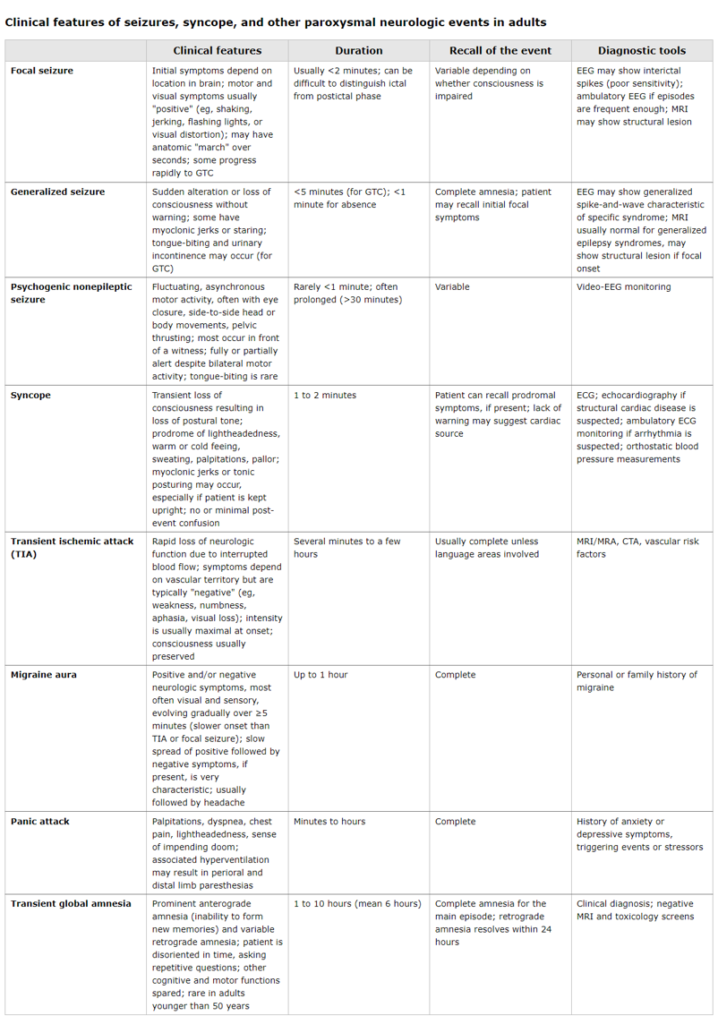
Seizure is only one cause of transient neurologic symptoms with or without alteration of consciousness. Other common causes of paroxysmal neurologic symptoms in adults are syncope, transient ischemic attack, migraine, and psychogenic nonepileptic seizures.
Diagnostic evaluation
Seizure is largely a clinical diagnosis made by history, physical and neurologic examinations, and selected additional tests to identify an underlying cause:
- A detailed description of the seizure should be obtained from the patient and witnesses and should include the circumstances leading up to the seizure, including possible triggers or precipitants, the ictal behaviors, and the postictal state.
- Prior similar events including subtle myoclonus or auras should not be overlooked in the history. Other items in the past medical history and a physical and neurologic examination are also important in the evaluation of a first seizure.
- Testing should include laboratory studies (electrolytes, glucose, calcium, magnesium, complete blood count, renal function tests, liver function tests, urinalysis, and toxicology screens), an electrocardiogram (ECG), an electroencephalogram (EEG) (urgently when impaired sensorium is persistent), and a neuroimaging study. Depending on the clinical situation, a lumbar puncture may also be indicated.
Seizure duration
Most seizures remit spontaneously within two minutes and rapid administration of a benzodiazepine or antiseizure medication is not required. Nonetheless, intravenous access is typically secured by paramedics or in the emergency department setting for patients presenting acutely so that medications can be administered if the seizure is more prolonged or recurs.
When to start antiseizure medication.
Antiseizure medications are not always indicated after a first seizure. The decision whether to start antiseizure medication therapy depends on multiple factors, including the probability that the event represented a seizure, the suspected or confirmed cause of the seizure based on the initial evaluation, the stability of the patient, and the estimated risk of recurrent seizure.
Indications for hospital admission
ASM: antiseizure medication.ASM started in consultation with neurology; treatment should be individualized.
¶ Consult with neurologist; continued ASM treatment may be warranted for patients with a higher risk of recurrent seizure (eg, those with encephalitis, hemorrhagic stroke, or other acute intracranial lesions).
Most patients with a first unprovoked seizure who have returned to their clinical baseline and have normal initial studies can be discharged from the emergency department with close outpatient follow-up. Hospitalization may be required for patients who have a first seizure associated with a prolonged postictal state or incomplete recovery. Other indications for hospitalization include status epilepticus, the presence of a systemic or neurologic illness or injury requiring additional evaluation and treatment, and questions regarding compliance.
Driving restrictions and other precautions
CNS: central nervous system; EEG: electroencephalography; ASM: antiseizure medication.Coexisting medical conditions likely to be worsened by a seizure (eg, osteogenesis imperfecta, shoulder reconstruction) may warrant treatment for low-risk patients.
¶ ASM decision made in consultation with neurology; treatment should be individualized; patient preference may reasonably lead high-risk patients to defer ASM until they have a second seizure.
All patients should be counseled about driving restrictions and other seizure precautions. Although specific regulations vary, the majority of states and countries require at least some period of abstinence from driving after a seizure or other event associated with loss or alteration of consciousness.
This algorithm summarizes our suggested approach to antiseizure treatment for convulsive status epilepticus (CSE) in adults. CSE is defined as a single unremitting seizure lasting >5 minutes or frequent clinical seizures without an interictal return to the baseline clinical state. Along with immediate antiseizure therapy, patients with CSE require simultaneous, rapid initiation of monitoring, including supportive care of airway, breathing, and circulation, and rapid recognition and treatment of hypoglycemia, electrolyte disturbance, poisoning, central nervous system infection, sepsis, and traumatic brain injury. The goal of therapy is to achieve seizure freedom (ie, cessation of clinical and electrographic seizures using continuous EEG). Refer to UpToDate topics on adult CSE for additional details.
Guideline | JAPANESE SOCIETY OF NEUROLOGY (neurology-jp.org)



