Normal pressure hydrocephalus characteristically presents with progressive gait impairment, cognitive deficits, and urinary urgency and/or incontinence.
Idiopathic normal pressure hydrocephalus (iNPH), a potentially reversible cause of dementia, is the most common form of hydrocephalus in adults. iNPH is a disorder of the elderly that characteristically presents with progressive gait impairment, cognitive deficits, and urinary urgency and/or incontinence (Hakim-Adams triad – classically described by Colombian neurosurgeon Salomon Hakim and R D Adams in 1965).
Gait disturbance with one additional feature is essential to consider the diagnosis; however, the clinical presentation requires further supportive assessment (i.e., imaging and cerebrospinal fluid (CSF) drainage) for confirmation. Some experts have challenged the term iNPH, as the intracranial pressure is not always normal in iNPH. The term idiopathic adult hydrocephalus syndrome (iAHS) has also been proposed.
Etiology
There are two forms of normal pressure hydrocephalus:
- Idiopathic (primary) NPH – There is no identifiable cause.
- Symptomatic (secondary) NPH – Cases with risk factors of earlier brain infection, hemorrhage, traumatic brain injury, or radiation contributing to hydrocephalus fall into this category.
Common features of iNPH and secondary normal pressure hydrocephalus are that both are communicating types of hydrocephalus and both carry a similar prognosis. The significant difference between them is that secondary NPH affects persons of all ages, while iNPH is mainly a disease of the elderly.
The basal intracranial pressure must be initially elevated for at least some period of time for NPH to develop.
Epidemiology
In the most extensive population-based study on the prevalence of iNPH done in Western Sweden, the research found that 0.2% among those in the age group 70 to 79 years and 5.9% of those 80 years of age and older matched guideline criteria for probable iNPH.
Most of the patients with iNPH were over 80 years of age. The average age of onset is approximately 70 years, and men and women are affected in equal numbers. iNPH is thought to account for roughly 6% of all cases of dementia. The estimated incidence of normal pressure hydrocephalus is 0.2 to 5.5 per 100000 person-years, and reports of its prevalence are 0.003% in persons under 65, and 0.2% to 2.9% for persons aged 65 or older.
Pathophysiology
The exact pathophysiologic pathway for iNPH remains unclear. But several mechanisms have been described leading to the development of the condition:
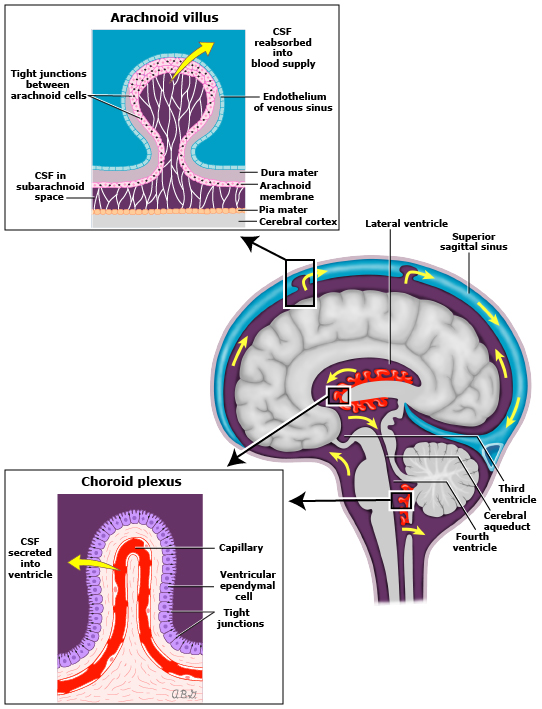
- The hyperdynamic flow of cerebrospinal fluid (CSF) in the aqueduct
- Reduced compliance of the subarachnoid space
- Increased CSF pulse pressure
- Reduced reabsorption of CSF in the venous system due to increased resistance
- Reabsorption of CSF through abnormal mechanisms like transependymal flow, rather than through Pacchionian granulations
- Cerebral blood flow reduction
- Altered expression of cerebrospinal fluid (CSF) tumor necrosis factor-alpha (which is known to regulate CSF production) and transforming growth factor-beta
- Failure of drainage of vasoactive metabolites (Silverberg 2004) – Abnormalities in CSF production and turnover may lead to a failed clearance of toxic molecules – an inability to clear amyloid-b peptides and tau protein could lead to an increase in their concentration in brain interstitial fluid, creating a potentially hostile environment for neuronal function and survival
- Loss of the Windkessel effect in the skull base arteries – The imbalance of CSF production and resorption is not due to overproduction but because of increased resistance to CSF outflow. The loss of elasticity of blood vessels may be either primary due to atherosclerosis or secondary due to low craniospinal compliance impeding the expansion of the skull base arteries. The increased brain pulsations result in higher compressive stress and shearing forces in the cerebral parenchyma. Due to the physical and physiological differences between superficial and deep (periventricular) brain tissue, the damage and loss start mainly in the periventricular areas as a result of cerebral auto-compression. This focal brain damage manifests as ventriculomegaly. The loss of the Windkessel effect also results in the lowering of cerebral blood flow, which leads to the simultaneous occurrence of iNPH and cerebral hypoperfusion; the latter, in turn, lowering CSF turnover.
Causes of gait abnormality
- The increased intracranial pressure leads to stretching and compression of the fibers of the corticospinal tract in the corona radiata that supply the legs, which pass in the close vicinity to the lateral ventricles as a result of interstitial edema
- Poor perfusion of periventricular white matter and prefrontal regions
- Compression of brainstem structures, such as the pedunculopontine nucleus
- Cause of dementia:
- As the ventricles continue to enlarge and the cortex pushes against the inner table of the calvarium, radial shearing forces lead to dementia.
Cause of bladder incontinence
- At an early stage, the periventricular sacral fibers of the corticospinal tract are stretched causing a loss of voluntary (supraspinal) control of bladder contractions (Gleason 1993); in later stages of the disease, dementia may contribute to incontinence (Corkill 1999).
- Also, in patients with iNPH, the role of comorbidities should be considered according to the International Society for Hydrocephalus and Cerebrospinal Fluid Disorder.[20][21] It is critical to rule out potential comorbidities that allow for the optimization of the patient’s care for each diagnosis, maximizing their clinical outcome.
Diagnostic evaluation
Diagnostic tests are required in the evaluation of patients with clinical evidence of NPH to exclude other conditions, to provide confirmation of the diagnosis, and to identify patients likely to respond to surgical intervention
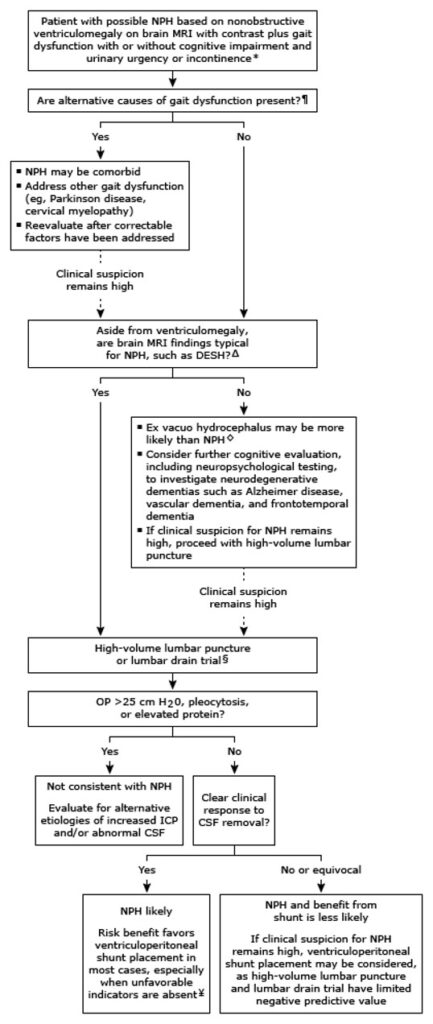
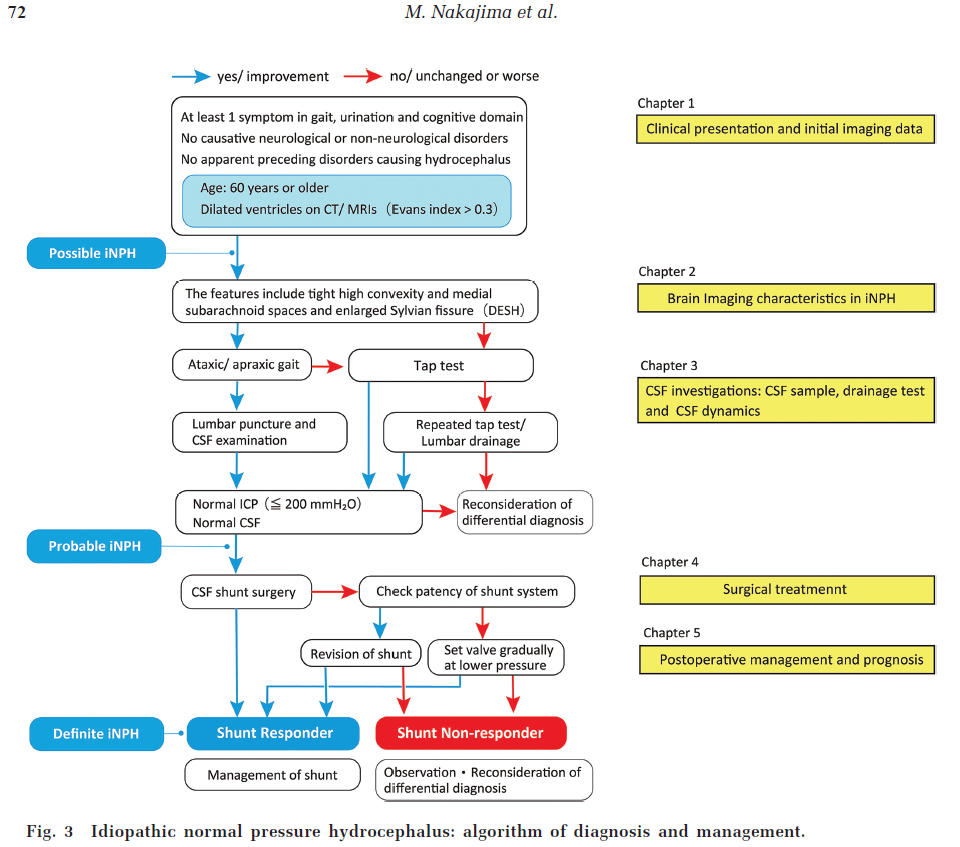
MRI: magnetic resonance imaging; DESH: disproportionately enlarged subarachnoid space hydrocephalus; OP: opening pressure; ICP: intracranial pressure; CSF: cerebrospinal fluid. Signs and symptoms of increased ICP, such as headaches, nausea/vomiting, papilledema, and visual loss, are not consistent with NPH and suggest an alternative diagnosis and need for additional evaluation beyond the scope of this algorithm. ¶ Examples include cervical or lumbar spondylosis, vestibular dysfunction, osteoarthritis, deconditioning, visual impairment, peripheral neuropathy, and medication side effects. Δ Typical neuroimaging findings for NPH include: Absent or modest cortical and hippocampal atrophy Disproportionately enlarged subarachnoid space hydrocephalus (DESH) Refer to UpToDate topic review on NPH for further additional details and imaging examples. ◊ Focally entrapped fluid in sulci, which is seen in DESH, should not be confused with cortical atrophy and ex vacuo hydrocephalus. § High-volume lumbar puncture is generally sufficient, although some clinicians and centers prefer lumbar drain trial. CSF should be analyzed for cell count, differential, total protein, and glucose. Refer to UpToDate topic reviews for additional details. ¥ Unfavorable prognostic factors for response to shunting include early appearance of cognitive impairment in relation to other symptoms, moderate to severe dementia, dementia present for >2 years, gait disorder absent or appearing after onset of dementia, alcoholism, marked white matter disease, and diffuse sulcal enlargement (cortical atrophy) and/or hippocampal atrophy.
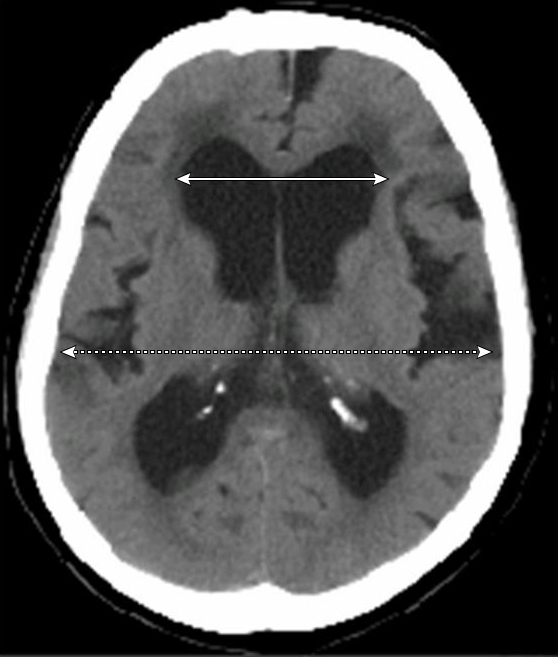
Axial CT image showing hydrocephalus and calculation of the Evans index. If the frontal horn measurement (arrow) as a ratio of the inner table of the skull (dashed arrow) is greater than 0.31, then the ventricles are enlarged.
 Cargando…
Cargando…
 Cargando…
Cargando…